Craft Is the Antidote to Slop.
From Genesis, man enters not a paradise without labor but a world of intentional creation. The LORD God places man in the Garden of Eden "to dress it and to keep it" (Genesis 2:15) establishing labor not as punishment but as sacred vocation. This original calling invites us to co-create the Kingdom, tending and developing the world with intention and care. Our fundamental purpose is not consumption but participation in the ongoing work of creation.
The serpent's temptation represents the first shortcut in human history."Ye shall be as gods" (Genesis 3:5) was not an invitation to deeper engagement with creation, but a way to get out of the work required to tend to it. The consequence wasn't the introduction of work itself, but its corruption into burdensome toil: "In the sweat of thy face shalt thou eat bread" (Genesis 3:19). Humanity's first sin was, in part, choosing the easy shortcut over the meaningful process – preferring effortless gain to the demanding but fulfilling work of tending the garden.
This first temptation remains alive today. Our post-enlightenment view that our world is purely material—that our lives are the outcome of physical processes devoid of feeling, craft, or meaning—is to discount the unique, historical, and stubbornly detailed nature of reality. This view misses what is evident: that the world we inhabit bears the marks of exacting, purposeful craftsmanship on both human and cosmic scales. Viewing the world as raw material is a cheap shortcut around the demanding, hermeneutic work of understanding the past and engaging deeply with the present.
The outputs of these shortcuts are Slop, the dominant cultural output of the twenty-first century. Slop emerges when we eliminate not just toil (the burdensome aspects of work) but labor itself (the meaningful human engagement with creation). Slop is production without history. Slop is detached from genuine human contribution. Slop born of effortless, replicable processes.
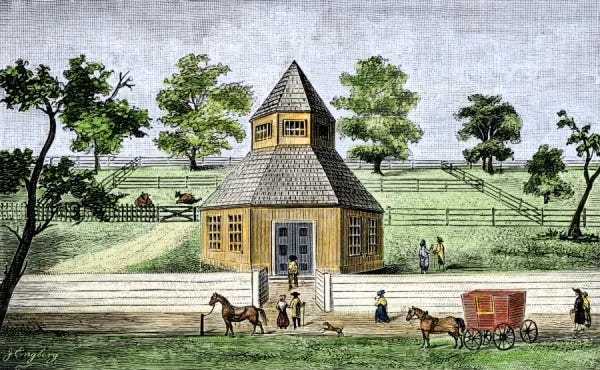
We see it in the overwhelming flood of AI-generated content on timelines. But slop is not just digital; it manifests physically in the uniform, history-denying aesthetic of new build transplant cities built from replicable templates, lacking any imprint of history or specific human interaction with place. It is also present in industrially farmed food that has seemingly never seen soil. This might explain why truly inspired creation, the antithesis of slop, often seems rooted in something beyond mere human effort or secular concern. Consider how no purely secular building has ever approached the grandeur of Chartres or any of the old cathedrals, and no secular music has reached the spiritual depth of Bach. Slop, in all its forms, is the result of attempting to conjure life and meaning without labor or place in history.
Language models provide the means for industrialization of Slop. In their highest calling, these tools can eliminate genuine toil: tending to burdensome emails, litigating with your co-op board, or drafting a parking ticket appeal. But when we ask a model to write a poem, design a church, or compose a eulogy, we get something fundamentally different from human creation. The model has never lost a loved one, never stood in a holy space, never lived. We can and should automate toil, but we must preserve craft. The difference is simple: when I use a model as leverage to remove toil, I remain source; when I ask a model to remove my agency by replacing my labor, something ancient and unseen becomes source.
Demons thrive in these automated realms. Not metaphorical demons, but the actual spiritual forces that have always sought to separate humanity from meaningful engagement with creation as we see in Genesis 3. The demonic recognizes in our shortcuts the perfect opportunity: tempt humans away from the difficult labor of making, growing, and building with our own hands and minds. Instead, offer an endless stream of effortless consumption—images without artists, music without musicians, stories without storytellers. The devil’s oldest strategy is, of course, promising godlike creation without godlike effort.
Yet, the biblical narrative does not end in the Garden lost to a shortcut. It culminates in Revelation with the vision of a city, the New Jerusalem (Revelation 21-22). This city is not a return to effortless paradise but a place whose jasper walls and river-lit avenues are inconceivable without millennia of labor and discovery – the accumulated craft and effort of humanity redeemed. The nations bring their "glory and honour into it" (Revelation 21:24), a glory that is the fruit of human labor and culture offered back to God. The perfected creation still involves ongoing fruitfulness and tending ("the tree of life... which bare twelve manner of fruits," Revelation 22:2). The Kingdom of God is not merely a distant future state but is, in a sense, present alongside us, requiring our active participation in building and tending it through meaningful labor. It is no coincidence that Christ was a carpenter and Moses a shepherd.
In this vision of redemptive labor, we can glimpse a more hopeful future where technology serves its highest purpose by eliminating true toil while preserving the sacred space for human hands and minds to engage in genuine craft. When automation frees us we gain capacity to redirect our energies toward the kinds of deeply human creative acts that build the Kingdom: tending gardens, raising cathedrals, composing hymns, and nurturing communities. It is a participation in the ongoing work of building the Kingdom.
Thank you Zack Baker, Nabeel Qureshi, Jeremy Giffon, Zoe Taylor, Toni Oloko, and Wolfgang Hammer for your feedback on various versions of these ideas and this piece.